Specialist Care for Gastrointestinal, Thyroid, Parathyroid & Adrenal Conditions
Adrenal Glands
What do the Adrenal Glands do?
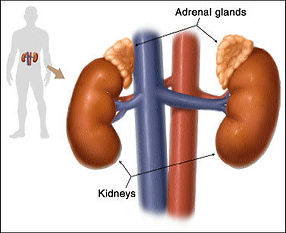
The adrenal glands are two pyramid shaped glands that sits on top of the kidneys like baseball caps. In broad terms, the adenal gland is made up of the cortex (outer shell) and the medulla (the core). They have completely different functions to the kidneys.
They are the stress glands of our body. As the name implies it makes a hormone called adrenaline and noradrenaline which essentially are responsible for the sensation you experience when nervous (eg. increase heart rate, pounding heart).
The adrenal glands also make a number of other hormones including cortisol, a hormone that controls how the body react to stress, androgens, a hormone that stimulates the development and maintenance of masculine characteristics and aldosterone, that regulates the body salt content and consequently the blood pressure. Like the thyroid gland the adrenal glands are also under the influence of the pituitary gland for some of its function (click `Adrenal Control system').
What does an Overactive Adrenal Gland mean?
Hormonal excess is often although not always due to a tumour or a growth in the adrenal gland. An overactive adrenal gland produces excess amount of one or more of the hormones that the adrenal gland normally produces resulting in disease states that are characteristics of the particular hormonal excess.
Cortisol excess: Known as Cushings syndrome/disease. Too much cortisol can result from excess production from the adrenal glands or from excess adrenocorticotrophin (ACTH) from the pituitary gland or an ACTH producing cancer (eg lung cancer). Symptoms of this is the same as people who have taken prolonged steroid therapy. Sufferers typically have upper body obesity, round faces, increased fat around the neck, and thin arms and legs. It has been increasingly recognised that a subgroup of patients may have excess production of cortisol but not to the level of developing overt Cushings disease. These patients often suffer from hypertension, diabetes and hyperlipidaemia (excess lipids). Left untreated a proportion of patients will continue to develop overt Cushings disease.
Aldosterone excess: Also known as hyperaldosteronism. Excess aldosterone may be produced from an abnormal adrenal gland or glands. Two types of abnormalities are seen: a benign tumour of one adrenal, called an adenoma, Conn's syndrome or a general enlargement of both adrenals, called bilateral adrenal hyperplasia. The result of this is in the majority of cases (60%) hypertension that may be accompanied with low potassium. A significant number of people may be completely asymptomatic.
Androgen excess: This hormone in excess can cause hirsutism which is excessive hair growth especially on the chin, lip, sideburns, breasts, sternum, the midline between the umbilicus and the pubis and the thigh. Severe acne and in extreme female cases, virilisation (male features) which is characterised by temporal balding, breast atrophy, clitoral enlargement, deepening of the voice, and extreme hirsutism.
Adrenaline and noradrenaline excess: Known as pheochromocytoma. The classical symptoms are those attributable to excess adrenaline production. Essentially sufferers will have recurring attacks of sweating, headache, nausea, vomiting, difficult to control hypertension, racing heart rate, tremors, chest or abdominal pains, headache and a feeling of high anxiety liken to impending death. Not infrequently sufferers may have been labeled to have panic attacks. Patients often have very high blood pressures that are difficult to control (requiring more than 4 blood pressure medications).
Can I get Underactive Adrenal glands?
Addison's disease occurs when the adrenal glands do not produce enough of the hormone cortisol and, in some cases the hormone aldosterone. The disease is also called adrenal insufficiency, or hypocortisolism. The disease is characterized by weight loss, muscle weakness, fatigue, low blood pressure, and sometimes darkening of the skin in both exposed and nonexposed parts of the body. Failure to produce adequate levels of cortisol can occur for different reasons. The problem may be due to a disorder of the adrenal glands themselves (primary adrenal insufficiency).
These include TB, chronic infection, mainly fungal infections, cancer cells spreading from other parts of the body to the adrenal glands, amyloidosis, surgical removal of the adrenal glands (Nelson's syndrome).
Alternatively, it can be due to inadequate stimulation by the pituitary gland (secondary adrenal insufficiency). This is easily treated by taking hormone replacement.
What do I do with this lump in my Adrenal gland?
Lumps in the adrenal gland can be discovered incidentally during routine CT scans for some other indication. We refer these lumps as adrenal incidentaloma. Two things to consider in the management of adrenal incidentalomas. First the size and secondly function. Essentially only 2% of tumours that are less than 4cm in its largest diameter are malignant. The risk of malignancy goes up to 25% as the size of tumour increase to >6cm. Using special measurements from the CT scan can only infer the nature of these growths. Without the evidence of metastases it is not possible to be 100% sure that the growth is benign or malignant. The second consideration is to determine whether the growth is functioning (making excess hormones) or non-functioning. Currently surgery is recommended for any tumours with a size greater than 4cm (3.5cm in <50yrs) or is functioning producing excess hormone (irrespect to size).
What treatments are available for Adrenal tumours?
Surgery is indicated when there is a discrete lesion producing excess hormones or for tumours greater than 4cm (3.5cm in the <50yrs). Laparoscopic surgery is the gold standard for adrenal tumours less than 6cm. Open surgery is reserved for larger tumours or when there are radiological suspicions of malignancy. With phaeochromocytoma, patients will have to take medicines to block the effects of adrenaline before embarking on surgery. In the case of Cushing's disease, extra supplements of steroids are given during the operation which is followed by a course of reducing dosages to allow the other adrenal gland to regain its function.
Surgery offers the only real prospect for cure for early adrenal cancers. In advance cancers, surgery offers debulking of the tumour giving chemotherapy a better chance to be effective.
What will happen after surgery or if I decline surgery?
Recovery following laparoscopic surgery is rapid and most patients will be discharged within 2 days of operation. It is not uncommon to find complete or improvement in hypertension, diabetes and obesity for conditions like phaeochromocytoma, overt/subclinical Cushing's disease and Conn's syndrome after surgery. In some cases long-term follow-up is required. For non-functioning adrenal incidentalomas that are less than 4cm that does not require surgery, it is advisable to have a repeat scan and functional screen to check for growth and development of hyperactivity after aperiod of time. Up to 20% of small tumours will grow and a similar proportion will develop hormonal hyperactivity.
